Dying Matters – raising public awareness
In 2008 the government published the End of Life Care Strategy for England, in which NCPC was invited to lead a national coalition to increase public awareness, discussion and debate around dying, death and bereavement. NCPC accepted the challenge and in 2009 the Dying Matters Coalition was born. In a short time the coalition has become established and respected and now boasts over 16,000 members. Whilst the Dying Matters Coalition’s main focus is England, we support and encourage better public awareness across the UK.
NCPC today
NCPC celebrated its 20th birthday in 2011 and is going from strength to strength. We produce a range of publications, leaflets, DVDs, conferences and training programmes to help our subscribers around the country deliver the best levels of care. We work with government, the NHS, the voluntary and private sectors to shape future strategies and plans. We involve patients, carers and families in everything we do to ensure our work is informed by people with real experience.
Is this a 'junior partner'? Who is in charge; who is controlling whom?
"There were two significant NICE consultations during the year, on an End of Life Care Quality Standard and on the use of strong opioids. Our consultation responses were informed by extensive feedback from our working groups as well as by people with personal experience of end of life care,and many of our key recommendations were accepted."
(NCPC Report and Financial Statements 31 March 2012)
What 'independence' is there here? This is a complex coalition of diverse but not dissimilar organisations, in close discussion, consultation, all sharing a like interest of mutual benefit: the promotion of the Integrated/Gold Standards/Dundee
NCPC appear to have a finger dipped in every bowl, just for tasters, of course. The umbrella seems more and more like a web...
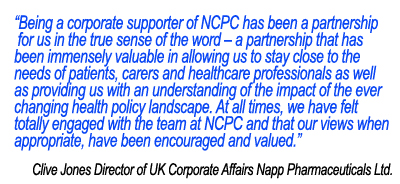
NCPC offers 'Corporate Partnerships', also.
One of these is Napp Pharmaceuticals -
NCPC appear to have a finger dipped in every bowl, just for tasters, of course. The umbrella seems more and more like a web...
NCPC offers 'Corporate Partnerships', also.
One of these is Napp Pharmaceuticals -
The NCPC has a sister organisation, the SPPC -
Services in
Click here to visit their website.
The web is as extensive in
This is SPPC. Comments follow after –
Liverpool care pathway for the dying patient
Page Updated 21.12.12
Misconceptions and inaccurate information about the Liverpool Care Pathway risk detracting from the substantial benefits it can bring to people who are dying and to their families. They may also cause unfounded anxiety and distress.
The hospice movement in the UK is famous around the world for looking after dying people with dignity and skill. Since the late 1990s, the Liverpool Care Pathway has been helping to spread elements of the hospice model of care into other healthcare settings, such as hospitals, care homes and people’s own homes.
The Liverpool Care Pathway:
- Requires staff ensure all decisions to either continue or to stop a treatment are taken in the best interest of each patient. It is not always easy to tell whether someone is very close to death – a decision to consider using the Liverpool Care Pathway should always be made by the most senior doctor available, with help from all the other staff involved in a person’s care. It should be countersigned as soon as possible by the doctor responsible for the person’s care.
- Emphasises that people should be involved in decisions about their care if possible and that carers and families should always be included in the decision-making process.
- Aims to prevent dying patients from having the distress of receiving treatment or tests that are not beneficial and that may in fact cause harm rather than good.
- Relies on staff being trained to have a thorough understanding of how to care for people who are in their last days or hours of life.
- Is continually evaluated in all the places where it is in use.
The Liverpool Care Pathway does not:
- Replace clinical judgement and is not a treatment, but a framework for good practice.
- Preclude the use of clinically assisted nutrition or hydration - it prompts clinicians to consider whether it is needed and is in the person’s best interest. GMC guidance (2010) provides specific information regarding this issue.
The Liverpool Care Pathway has been suggested as a model of good practice in the last hours and days of life by UK, English and Scottish national policy frameworks, including Living and Dying Well, the Scottish government’s national action plan for palliative and end of life care published in 2008. The General Medical Council published guidance on treatment and care towards the end of life in 2010 and the principles that underpin the Liverpool Care Pathway are consistent with that guidance.
The Liverpool Care Pathway is not in any way about ending life, but rather about supporting the delivery of excellent end of life care, to the benefit of patients and their families.
Statements of Support for the Use of the Liverpool Care Pathway
In the light of inaccurate and misleading media coverage about the Liverpool Care Pathway a number of organisations and individuals have made statements supporting the appropriate use of the pathway here
Other Resources
This is a link to an editorial on the Liverpool Care Pathway written by Kirsty Boyd and Scott Murray of Edinburgh University, published in the BMJ.http://bmj.com/cgi/content/full/bmj.e7718
Link to GMC guidance and supporting materials for doctors: http://www.gmc-uk.org/guidance/ethical_guidance/end_of_life_care.asp
Answers to some frequently asked questions on this topic - here


No comments:
Post a Comment